High-performing medical practice reach success with more than just best practices — they measure key performance indicators (KPIs) and benchmark against other organizations to understand where they can improve and sustain that excellence.
During a recent MGMA member-exclusive webinar, MGMA’s Andrew Hajde, CMPE, director of content and consulting, and Ashley Ager, MSM, organizational membership account manager, detailed how measurement and tracking of specific metrics can inform decision-making that leads to being a better-performing practice.
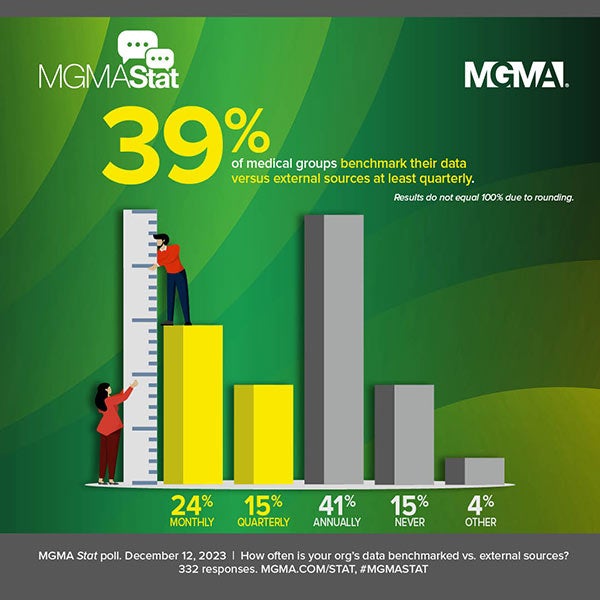
This type of data work has shown over time to be valuable and widely used in the industry: More than 8 in 10 healthcare leaders report using benchmarking data to address issues in their businesses, as it allows administrators and other medical group leaders to transform data into action.
“Better performers blend new skills and perspectives for better outcomes while keeping a close eye on the well-being of clinicians and staff in their roles as leaders,” Ager said. MGMA’s DataDive surveys track this through the Better Performers data set, which covers survey data from more than 4,000 medical groups to highlight top performance in the areas of operations, profitability, productivity and value.
In key areas such as productivity and expenses, benchmarking data year over year can quickly tell the story of what is happening in an individual clinic, a broader group or even the entire industry.
Case in point: the MGMA DataDive Cost and Revenue data set offers benchmarks for total encounters per full-time-equivalent (FTE) physician (Table 1) that, trended over time, help reveal how different ownership models fared from pre-COVID-19 pandemic years to recovery.

The same data set also reveals benchmarks for total medical revenue per FTE physician (Table 2) which — when trended across one and three years, respectively — give a sense for how different specialties and ownership structures fared in their pandemic recovery.

“These [benchmarks] really can help you make decisions … on where you really need to focus your attention for making improvements for the future,” Hajde said.
Learning from data
Deciding on which KPIs to track will enable operational and workflow changes in certain scenarios, as Hajde outlined:
- Patient access — a major concern amid limited staffing and the need to sustain revenue — should be tracked by same-day appointment availability and time to third-next-available appointment (TNAA), with reviews of visit types of appointment durations.
- To address staffing shortages, cross-training and optimization of advanced practice providers (APPs) can be used in conjunction with benchmarks for hiring and retention incentives to ensure your compensation is competitive.
“We're also seeing many practices utilizing nontraditional clinical staff that we wouldn't have always seen in a practice setting: CNAs, EMTs, and others to help them out, especially in those areas across the country where they can't find medical assistants (MAs) and or can't retain people,” Hajde said. “Using staffing benchmarks to see what ratios you should be having per physician FTE and other information [helps you] make really wise decisions based on what others are doing in your specialty.”
Ager echoed the staffing difficulties, noting that medical practices can “get creative and invest in tools that deepen an MA’s connection to the patient care,” such as disease-specific, care-enabled pathways “that empower the MAs to identify patients who need expedited care.
In one group where this approach helped MAs ask the right questions in order to identify patients at higher risk, the time spent by physicians reviewing patient data went down by 10 to 15 minutes per patient. “In some cases, that can be an entire added patient to the provider schedule,” Ager noted.
Ager also offered the example of a urology group using a method to identify patients with chronic cystitis who would benefit from a remote cystitis clinic. “When patients would present with symptoms, the MA would order lab tests to identify microbial DNA, RNA urine,” Ager said. “This approach would prove to be more effective in treating UTIs and patients with cystitis than traditional urine dipstick analysis,” as the remote clinic was able to help more than 100 patient avoid urgent or emergency care in a year, while also generating almost $70,000 in revenue for chronic care management.
Revenue cycle management
Focusing on revenue cycle optimization amid rising costs and reimbursement challenges is a top priority for most medical groups in 2023, and using data to make operational decisions in this domain is another important piece of your benchmarking and KPI tactics, Ager said.
Use of a claims scrubbing tool and using best practices in coding, documentation and denials management all aid in improving days in A/R, but it also requires dedication to running reports on these metrics — at least monthly for administrative leaders and more frequently for billers.
Ager added that technological tools such as automated check-in, prompts for balances, and methods for patients to enter their demographic and insurance information before a visit are some of the top ways for practices to become more efficient and avoid errors that can lead to bad debt and unnecessary write-offs.
“A lot of our Better Performers collect more A/R in the first 30 days as compared to the industry benchmark,” Ager said, underscoring the usefulness of creating scripts for your front office staff to have proactive conversations with patients about payments.
Code-specific benchmarking
Hajde emphasized that several survey data sets often have a wealth of benchmarks that might fly under a user’s radar and be underutilized, such as the MGMA DataDive Procedural Profile data set, which allows users to do CPT®-level benchmarking.
Whether you’re in orthopedic surgery, cardiology or some other specialty, this tool can help you look at all of the CPT® codes submitted in those specialties. Not only can you find typical CPT® code average volume — you can also see exactly what is being billed for a typical clinician and the associated volumes of each code. You can see what specialties are expanding their services, such as CPT® codes that were traditionally performed by dermatologists or plastic surgeons expanding into other specialties, or even the volumes of each type of new and traditional surgical procedure a heart surgeon or other specialist is performing. You can even filter this data by ownership type, geographic location and many other factors to see the specific segment you want.
Data visualization

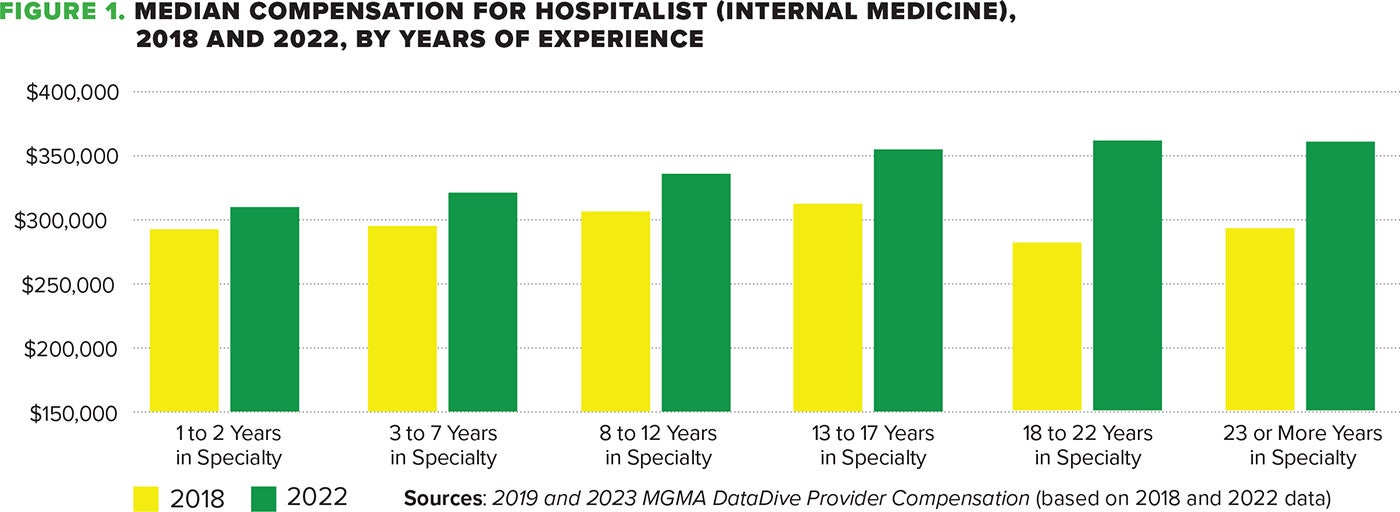
Another important tool to use in your data work is the Pay-to-Production Plotter, which visualizes the relationship between data, such as provider compensation and productivity (see Figure 1), and help validate findings and make decisions about physician compensation plan changes.
“This is particularly useful when you have part-time physicians who are paid solely on a compensation-per-work-RVU basis,” Ager said. “It's a great illustration of where physicians’ compensation and productivity lines up with MGMA’s actual respondents within the same specialty … and it helps you identify your outliers and keep track of them.” This plotter is often used in conjunction with fair market valuations of physician compensation for medical groups, hospitals, health systems.
Top operational and billing/RCM KPIs
The following operational KPIs are important for practice leaders to track and analyze on a regular basis:
- Physician/APP wRVU productivity
- Physician/APP total encounters
- Physician/APP panel size
- Physician/APP FTE status [i.e., full-time (1.0/40 hours), part-time (0.5/20hours)]
- CPT® codes (E/M and total procedures)
- FTE staffing ratios for clinical/nonclinical staff by location
- Including provider to nonprovider ratios
- Patient portal use
- Wait times (throughput)
- Same-day appointments
- Third-next-available appointments (By type – new/established)
- No-show rates
- Cancellation rates
- Turnover/retention rate
- Phone call stats (including volume, length, abandonment rate)
- Patient satisfaction scores (Blended top box)
The following billing and revenue cycle KPIs are also recommended for regular tracking and analysis:
- Total medical revenue after operating costs
- Gross revenues
- Net fee-for-service (FFS) or other net revenues
- Collection ratios/average reimbursement rate
- Claims denial rates and denial write-offs
- Bad debt
- Payer mix
- A/R days and A/R aging comparisons (by bucket: 0-30, 31-60, 61-90, 91-120, 120+ days)
- Charge posting and billing lag time
- Copay collections
- Patient-due collections
- CPT® codes (E/M comparison to CMS/MGMA Procedural Profile and procedures)
- Physician/APP wRVU productivity
Attendees of the webinar noted that they typically will review which KPIs they are tracking either quarterly or annually to ensure the right metrics are being reported and then reviewed in some combination of data visualization software, web-based tool, EHR-embedded tool or commercially available RCM tools, such as MGMA DataDiscovery. Finding the right combination for your specific situation is crucial, Hajde noted.
“The more you can automate, where you don't have to have so much manual labor on a monthly basis or quarterly basis … makes this so much easier to do,” Hajde said.
Ultimately, helping others within the organization understand why these benchmarks are important will be a factor in the overall success of your efforts, as well as seeking input from others about what it is being measured and analyzed.
“Gathering input from your team members is going to make them feel valued and make them feel part of this change,” Ager said. “That’s going to increase the chances of long-term success. … Make sure you clearly communicate the reasons for the change, the expected outcomes, and the steps that need to be taken to implement this change.”
Learn more
- Medical Practice Evaluation Tool: This self-paced tool helps determine how your practice’s operations stack up against top performers, with each domain of the Body of Knowledge represented.
- MGMA Advance: A member-benefit online assessment includes a 90-question review of your industry knowledge, providing a customizable pathway for your individual education needs.
- MGMA DataDive: Thousands of metrics allowing you to see the best in your organization and your areas for improvement.
- MGMA DataDiscovery: An intelligent medical group analytics tools designed to review and analyze your physician practice performance.